Treatment for Plantar Fasciitis
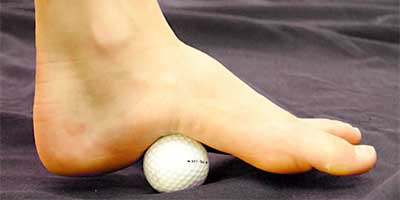
In part one, plantar fasciitis was identified as a painful condition on the bottom of the heel. This article explores treatment options. In any injury always use the RICE mnemonic: Rest, Ice, Compress and Elevate. Plantar fasciitis is a painful,…

